Seizure
| Epileptic seizure | |
|---|---|
| Other names | Epileptic fit,[1] seizure, fit, convulsions[2] |
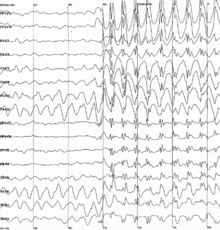 | |
| Generalized 3 Hz spike and wave discharges in an electroencephalogram (EEG) of a patient with epilepsy | |
| Specialty | Neurology, emergency medicine |
| Symptoms | Variable[3] |
| Complications | Falling, drowning, car accidents, pregnancy complications, emotional health issues[4] |
| Duration | Typically < 2 minutes[5] |
| Types | Focal, generalized; Provoked, unprovoked[6] |
| Causes | Provoked: Low blood sugar, alcohol withdrawal, low blood sodium, fever, brain infection, traumatic brain injury[3][6] Unprovoked: Flashing Lights/Colors Unknown, brain injury, brain tumor, previous stroke[6][7][3] |
| Diagnostic method | Based on symptoms, blood tests, medical imaging, electroencephalography[7] |
| Differential diagnosis | Syncope, psychogenic non-epileptic seizure, migraine aura, transient ischemic attack[3][8] |
| Treatment | Less than 5 min: Place person on their side, remove nearby dangerous objects More than 5 min: Treat as per status epilepticus[3][5][9] |
| Frequency | ~10% of people (overall worldwide lifetime risk)[10][11] |
A seizure is a sudden change in behavior, movement, and/or consciousness due to abnormal electrical activity in the brain.[3][6] Seizures can look different in different people. It can be uncontrolled shaking of the whole body (tonic-clonic seizures) or a person spacing out for a few seconds (absence seizures).[3][12][8] Most seizures last less than two minutes.[5] They are then followed by confusion/drowsiness before the person returns to normal.[3][8] If a seizure lasts longer than 5 minutes, it is a medical emergency (status epilepticus) and needs immediate treatment.[3][5][9]
Seizures can be classified as provoked or unprovoked.[3][6] Provoked seizures have a cause that can be fixed, such as low blood sugar, alcohol withdrawal, high fever, recent stroke, and recent head trauma.[3][6] Unprovoked seizures have no clear cause or fixable cause.[3][6][7] Examples include past strokes, brain tumors, brain vessel malformations, and genetic disorders.[3] If no cause is found, it is called an idiopathic seizure.[5][13] After a first unprovoked seizure, the chance of experiencing a second one is about 40% within 2 years.[5][14] People with repeated unprovoked seizures are diagnosed with epilepsy.[5][6]
Doctors assess a seizure by first ruling out other conditions that look similar to seizures, such as fainting and strokes.[3][8] This includes taking a detailed history and ordering blood tests.[3][13] They may also order an electroencephalogram (EEG) and brain imaging (CT and/or MRI).[3][7] If it is a person's first seizure and it was "provoked", or caused by another condition, treatment of the cause is usually enough to treat the seizure.[3] If the seizure is "unprovoked", brain imaging is abnormal, and/or EEG is abnormal, start anti-seizure medications is generally recommmended.[3][7][14]
Signs and symptoms
[edit]A seizure can last from a few seconds to 5 minutes.[5] Once it reaches and passes 5 minutes, it is known as status epilepticus.[3][5][9] Accidental urination (urinary incontinence), stool leaking (fecal incontinence), tongue biting, foaming of the mouth, and turning blue due to inability to breathe commonly are seen in seizures.[3][8]
A period of confusion typically follows the seizure that lasts from seconds to hours before a person returns to normal. This period is called a postictal period.[15] Other symptoms during this period include drowsiness, headache, difficulty speaking, psychosis, and weakness.[15][16][17]
Observable signs and symptoms of seizures vary depending on the type.[3][13] Seizures can be classified into generalized seizures and focal seizures, depending on what part of the brain is involved.[3][13]
Focal seizures
[edit]Focal seizures affect a specific area of the brain, not both sides.[13] It may turn into a generalized seizure if the seizure spreads through the brain.[3][13][8] Consciousness may or may not be impaired.[3][5] The signs and symptoms of these seizures depends on the location of the brain that is affected. Focal seizures usually consist of motor symptoms or sensory symptoms.[3]
- Sensory symptoms: Auras are subjective sensations that occur before focal seizures. Auras include changes in vision, hearing, or smell (example is smelling rubber).[3][13][18] Feelings of deja-vu or abdominal discomfort are also examples of auras.[3][13] A person who experiences focal weakness of a limb may also have just experienced a focal seizure. This is known as Todd's paralysis.[3][13][19]
- Motor symptoms: Head turning and eyes moving to one side, with contraction of limbs on one side is a common presentation.[13] Automatisms are also an indicator that a seizure is focal.[3][5] These are repetitive movements. It can be lip smacking, chewing, swallowing, eyelid fluttering, feet shuffling, or picking movements.[5] Jacksonian March is also a motor presentation of a focal seizure, with contractions spreading from one muscle to the next on one side of the body.[13][5]
Generalized seizures
[edit]Generalized seizures affect both sides of the brain and typically involve both sides of the body.[3] They all involve a loss of consciousness and usually happen without warning.[3][13] There are six main types of generalized seizures: tonic-clonic, tonic, clonic, myoclonic, absence, and atonic seizures.[3]
- Tonic-clonic seizures, also known as Grand Mal seizures, present with continuous stiffening of the body for 10–20 seconds followed by rhythmic jerking.[8][13] It may be accompanied by an increased in blood pressure, increase in heart rate, urinary incontinence.[8][5] The person may turn blue if breathing is impaired.[8][5] Shoulder dislocation and tongue biting are also possible.[8][13]
- Tonic seizures produce constant contractions of the muscles. The body stiffens for a prolonged period of time.[3] The muscles most commonly affected are the neck, shoulders, hips, and trunk.[5]
- Clonic seizures involve jerking of the muscles rhythmically.[5]
- Myoclonic seizures involve short contractions of muscles in either a few areas of the body or through the whole body. They are not typically rhythmic.[5]
- Absence seizures last 10–15 seconds usually.[5][8] It is characterized by a sudden, brief episode where a person is unaware of what is happening and does not respond.[8] The person stops in the middle of activity.[8] The person often does not fall over. They may return to normal right after the seizure ends, with no postictal state.[8][5] The person is usually unaware of what just happened.
- Atonic seizures involve the loss of muscle activity causing a person to drop abruptly with their muscles limp.[3][5] This is called a drop attack.[5]
Causes
[edit]Seizures have a number of causes. Seizures can be classified into provoked or unprovoked.[3] Provoked seizures have a cause that is temporary and reversible.[3] They are also known as Acute Symptomatic Seizures as they occur closely after the injury.[20] Unprovoked seizures do not have a known cause or the cause is not reversible.[3] Unprovoked seizures are typically considered epilepsy and treated as epilepsy.[3][8] Of those who have a seizure, about 25% have epilepsy.[21] Those with epilepsy may have certain triggers that they know cause seizures to occur, including emotional stress, sleep deprivation, and flickering lights.[5]
Causes of provoked seizures
[edit]Metabolic
[edit]Dehydration can trigger epileptic seizures by changing electrolyte balances.[22] Low blood sugar, low blood sodium, high blood sugar, high blood sodium, low blood calcium, high blood urea, and low blood magnesium levels may cause seizures.[3][5][22]
Medications
[edit]Up to 9% of status epilepticus cases occur due to drug intoxication.[23] Common drugs involved include antidepressants, stimulants (cocaine), and antihistamines.[23] Withdrawal seizures commonly occur after prolonged alcohol or sedative use.[3][23] In people who are at risk of developing epileptic seizures, common herbal medicines such as ephedra, ginkgo biloba and wormwood can provoke seizures.[24]
Acute infections
[edit]Systemic infection with high fever is a common cause of seizures, especially in children.[3][25] These are called febrile seizures and occur in 2–5% of children between the ages of six months and five years.[26][25] Acute infection of the brain, such as encephalitis or meningitis are also causes of seizures.[3]
Acute brain trauma
[edit]Acute stroke or brain bleed may lead to seizures.[3] Stroke is the most common cause of seizures in the elderly population.[27] Post-stroke seizures occur in 5-7% of those with ischemic strokes.[28] It is higher in those who experienced brain bleeds, with 10-16% risk in those patients.[28] Recent traumatic brain injury may also lead to seizures. 1 to 5 of every 10 people who have had traumatic brain injury have experienced at least one seizure.[29] Seizures may occur within 7 days of the injury (early posttraumatic seizure) or after 7 days have passed (late posttraumatic seizure).[29]
Causes of unprovoked seizures
[edit]Structural
[edit]Space-occupying lesions in the brain (abscesses, tumours) are one cause of unprovoked seizures.[3] In people with brain tumours, the frequency of epilepsy depends on the location of the tumor in the cortical region.[30] Abnormalities in blood vessels of the brain (Arteriovenous malformation) can also cause epilepsy.[3] In babies and children, congenital brain abnormalities, such as lissencephaly or polymicrogyria, will also result in epilepsy.[3][31] Hypoxic-ischemic encephalopathy in newborns will also predispose the newborn to epilepsy.[32]
Prior brain trauma
[edit]Strokes, brain bleeds, and traumatic brain injury can all also lead to epilepsy if seizures re-occur. If the first seizure occurs more than 7 days following a stroke, there is a higher chance of the person developing epilepsy.[27] Post-stroke epilepsy accounts for 30%-50% of new epilepsy cases.[27] This is also the case for traumatic brain injury, with 80% of people with late posttraumatic seizures having another seizure occur, classifying it as epilepsy.[29]
Prior brain infections
[edit]Infections of newborns that occur while before or during birth, such as herpes simplex virus, rubella, and cytomegalovirus, all carry a risk of causing epilepsy.[33] Infection with the pork tapeworm, which can cause neurocysticercosis, is the cause of up to half of epilepsy cases in areas of the world where the parasite is common.[33][34] Meningitis and encephalitis also carry the risk of causing long-term epilepsy as well.[3][33]
Genetic epilepsy syndromes
[edit]During childhood, well-defined epilepsy syndromes are generally seen. Examples include Dravet Syndrome, Lennox-Gastaut Syndrome, and Juvenile Myoclonic Epilepsy.[3]
Mechanism
[edit]Neurons function by either being excited or inhibited.[35] Excited neurons fire electrical charges while inhibited neurons are prevented from firing.[35] The balance of the two maintains our central nervous system.[35] In those with seizures, neurons are both hyperexcitable and hypersynchronous, where many neurons fire numerously at the same time.[36] This may be due to an imbalance of excitation and inhibition of neurons.[37][38][36]
γ-aminobutyric acid (GABA) and Glutamate are chemicals called neurotransmitters that work by opening or closing ion channels on neurons to cause inhibition or excitability.[38][39] GABA serves to inhibit neurons from firing. It has been found to be decreased in epilepsy patients.[38][37] This may explain the lack of inhibition of neurons resulting in seizures.[38][37] Glutamate serves to excite neurons into firing when appropriate.[38] It was found to be increased in those with epilepsy.[38][37] This is a possible mechanism for why there is hyper-excitability of neurons in seizures.
Seizures that occur after brain injury may be due to the brain adapting to injury (neuroplasticity).[40] This process is known as epileptogenesis.[41] There is loss of inhibitory neurons because they die due to the injury.[41][40] The brain may also adapt and make new neuron connections that may be hyper-excitatory.[41][40]
Brief seizures, such as absence seizures lasting 5–10 seconds, do not cause observable brain damage.[42] More prolonged seizures have a higher risk of neuronal death.[42] Prolonged and recurrent seizures, such as status epilepticus, typically cause brain damage.[42] Scarring of brain tissue (gliosis), neuronal death, and shrinking of areas of the brain (atrophy) are linked to recurrent seizures.[42][43] These changes may lead to the development of epilepsy.[43]
Diagnosis
[edit]
Diagnosis of seizures involve gathering history, doing a physical exam, and ordering tests. These are done to classify the seizure and determine if the seizure is provoked or unprovoked.[3][5]
History and Physical Examination
[edit]
Events leading up to the seizure and what movements occurred during the seizure are important in classifying the type of seizure.[3][5] The person's memory of what happened before and during the seizure is also important. However, since most people that experience seizures do not remember what happened, it is best to get history from a witness when possible.[5][44] Video recording of the seizure is also helpful in diagnosis of seizures.[5] Events that occurred after the seizure are also an important part of the history.[5] Past medical history, such as past head trauma, past strokes, past febrile seizures, or past infections, are helpful.[5] In babies and children, information about developmental milestones, birth history, and previous illnesses are important as potential epilepsy risk factors.[5] Family history of seizures is also important in evaluating risk for epilepsy.[5] History regarding medication use, substance use, and alcohol use is important in determining a cause of the seizure.[3][5][44]
Most people are in a postictal state (drowsy or confused) following a seizure.[15] A bite mark on the side of the tongue or bleeding from the mouth strongly indicates a seizure happened.[8][44] But only a third of people who have had a seizure have such a bite.[45] Weakness of one limb or asymmetric reflexes are also signs a seizure just occurred.[8][5][44] Presence of urinary incontinence or fecal incontinence also strongly suggests a seizure occurred.[8] However, most people who have had a seizure will have a normal physical exam.[5]
Tests
[edit]
Blood tests can determine if there are any reversible causes of the seizure (provoked seizures).[3][44] This includes a complete blood count that may show infection.[8][44] A comprehensive metabolic panel is ordered to rule out abnormal sugar levels (hypoglycemia or hyperglycemia) or electrolyte abnormalities (such as hyponatremia) as a cause.[8][44] A lumbar puncture is mainly done if there is reason to believe infection or inflammation of the nervous system is occurring.[3][44] Toxicology screening is also mainly done if history is suggestive.[5][44]
Brain imaging by CT scan and MRI is recommended after a first seizure, especially if no provoking factors are discovered.[5][3] It is done to detect structural problems inside the brain, such as tumors.[5] MRI is generally the better imaging test, but CT scan is preferred when intracranial bleeding is suspected.[7] Imaging may be done at a later point in time in those who return to their normal selves while in the emergency room.[7]
An electroencephalography (EEG) measures the brain's electrical activity.[46] It is used in cases of first seizures that have no provoking factor, normal head imaging, and no prior history of head trauma.[3] It will help determine the type of seizure or epilepsy syndrome present, as well as where the seizures are coming from if its focal.[3][5] It is also used when a person has not returned to baseline after a seizure for a prolonged time.[3]
Differential diagnosis
[edit]Other conditions that commonly get mistaken for a seizure include syncope, psychogenic nonepileptic seizures, cardiac arrhythmias, migraine headaches, and stroke/transient ischemic attacks.[3][5]
Prevention
[edit]There are times when a person has never had a seizure but anti-seizure medications are started to prevent seizures in those at risk.[3] Following traumatic brain injury, anti-seizure medications decrease the risk of early seizures but not late seizures.[47][48] However, there is no clear evidence that anti-seizure medications are effective at preventing seizures following brain surgery (craniotomy), a brain bleed, or after a stroke.[49][50][51][52][53]
Prevention of seizures from re-occurring after a first seizure depends on many factors. If it was an unprovoked seizure with abnormal brain imaging or abnormal EEG, then it is recommended to start anti-seizure medication.[3] If a person has an unprovoked seizure, but physical exam is normal, EEG is normal, and brain imaging is normal, then anti-seizure medication may not be needed.[3] The decision to start anti-seizure medications should be made after a discussion between the patient and doctor.
In children with one simple febrile seizure, starting anti-seizure medications is not recommended.[3][54] While both fever medications (antipyretics) and anti-seizure medications reduce reoccurrence, the harmless nature of febrile seizures outweighs the risks of these medications.[54] However, if it was a complex febrile seizure, EEG should be done. If EEG is abnormal, starting prophylactic anti-seizure medications is recommended.[3]
Management
[edit]During an active seizure, the person seizing should be slowly laid on the floor.[55] Witnesses should not try to stop the convulsions or other movements.[55] Potentially sharp or dangerous objects should be moved from the area around a person experiencing a seizure so that the individual is not hurt.[55] Nothing should be placed in the person's mouth as it is a choking hazard.[55] After the seizure, if the person is not fully conscious and alert, they should be turned to their side to prevent choking. This is called recovery position.[55] Timing of the seizure is also important. If a seizure is longer than five minutes, or there are two or more seizures occurring in five minutes, it is a medical emergency known as status epilepticus.[9][56] Emergency services should be called.
Medication
[edit]The first line medication for an actively seizing person is a benzodiazepine, with most guidelines recommending lorazepam.[3][57] Diazepam and midazolam are alternatives.[3] It may be given in IV if emergency services is present.[3] Rectal and intranasal forms also exist if a child has had seizures previously and was prescribed the rescue medication.[58] If seizures continue, second-line therapy includes phenytoin, fosphenytoin, and phenobarbital.[3] Levetiracetam or valproate may also be used.[3]
Starting anti-seizure medications is not typically recommended if it was a provoked seizure that can be corrected.[3] Examples of causes of provoked seizures that can be corrected include low blood sugar, low blood sodium, febrile seizures in children, and substance/medication use. Starting anti-seizure medications is usually for those with medium to high risk of seizures re-occurring. This includes people with unprovoked seizures with abnormal brain imaging or abnormal EEG.[3][5] It also includes those who have had more than one unprovoked seizure more than 24 hours apart.[3][59]
It is recommended to start with one anti-seizure medication.[5][59] Another may be added if one is not enough to control the seizure occurrence.[59] Approximately 70% of people can obtain full control with continuous use of medication.[60] The type of medication used is based on the type of seizure.[5][59]
Anti-seizure medications may be slowly stopped after a period of time if a person has just experienced one seizure and has not had anymore.[5] The decision to stop anti-seizure medications should be discussed between the doctor and patient, weighing the benefits and risks.
Surgery
[edit]In severe cases where seizures are uncontrolled by at least two anti-seizure medications, brain surgery can be a treatment option.[5][59] Epilepsy surgery is especially useful for those with focal seizures where the seizures are coming from a specific part of the brain.[59] The amount of brain removed during the surgery depends on the extent of the brain involved in the seizures. It can range from just removing one lobe of the brain (temporal lobectomy) to disconnecting an entire side of the brain (hemispherectomy).[5] The procedure can be curative, where seizures are eliminated completely.[5] However, if it is not curative, it can be palliative that reduces the frequency of seizures but does not eliminate it.[61]
Other
[edit]Helmets may be used to provide protection to the head during a seizure. Some claim that seizure response dogs, a form of service dog, can predict seizures.[62] Evidence for this, however, is poor.[62] Cannabis has also been used for the management of seizures that do not respond to anti-seizure medications. Research on its effectiveness is ongoing, but current research shows that it does reduce seizure frequency.[63][64] A ketogenic diet or modified Atkins diet may help in those who have epilepsy who do not improve following typical treatments, with evidence for its effectiveness growing.[65][66]
Precautions
[edit]Following a person's first seizure, they are legally not allowed to drive until they are seizure-free for a period of time.[3] This period of time varies between states, but is usually between 6 and 12 months.[3][7] They are also cautioned against working at heights and swimming alone in case a seizure occurs.[3]
Prognosis
[edit]Following a first unprovoked seizure, the risk of more seizures in the next two years is around 40%.[5][14] Starting anti-seizure medications reduces recurrence of seizures by 35% within the first two years.[44] The greatest predictors of more seizures are problems either on the EEG or on imaging of the brain.[3][5] Those with normal EEG and normal physical exam following a first unprovoked seizure had less of risk of recurrence in the next two years, with a risk of 25%.[5] In adults, after 6 months of being seizure-free after a first seizure, the risk of a subsequent seizure in the next year is less than 20% regardless of treatment.[67] Those who have a seizure that is provoked have a low risk of re-occurrence, but have a higher risk of death compared to those with epilepsy.[68]
Epidemiology
[edit]Approximately 8–10% of people will experience an epileptic seizure during their lifetime.[69] In adults, the risk of seizure recurrence within the five years following a new-onset seizure is 35%; the risk rises to 75% in persons who have had a second seizure.[69] In children, the risk of seizure recurrence within the five years following a single unprovoked seizure is about 50%; the risk rises to about 80% after two unprovoked seizures.[70] In the United States in 2011, seizures resulted in an estimated 1.6 million emergency department visits; approximately 400,000 of these visits were for new-onset seizures.[69]
History
[edit]Epileptic seizures were first described in an Akkadian text from 2000 B.C.[71] Early reports of epilepsy often saw seizures and convulsions as the work of "evil spirits".[72] The perception of epilepsy, however, began to change in the time of Ancient Greek medicine. The term "epilepsy" itself is a Greek word, which is derived from the verb "epilambanein", meaning "to seize, possess, or afflict".[71] Although the Ancient Greeks referred to epilepsy as the "sacred disease", this perception of epilepsy as a "spiritual" disease was challenged by Hippocrates in his work On the Sacred Disease, who proposed that the source of epilepsy was from natural causes rather than supernatural ones.[72]
Early surgical treatment of epilepsy was primitive in Ancient Greek, Roman and Egyptian medicine.[73] The 19th century saw the rise of targeted surgery for the treatment of epileptic seizures, beginning in 1886 with localized resections performed by Sir Victor Horsley, a neurosurgeon in London.[72] Another advancement was that of the development by the Montreal procedure by Canadian neurosurgeon Wilder Penfield, which involved use of electrical stimulation among conscious patients to more accurately identify and resect the epileptic areas in the brain.[72]
Society and culture
[edit]Economics
[edit]Seizures result in direct economic costs of about one billion dollars in the United States.[7] Epilepsy results in economic costs in Europe of around €15.5 billion in 2004.[74] In India, epilepsy is estimated to result in costs of US$1.7 billion or 0.5% of the GDP.[60] They make up about 1% of emergency department visits (2% for emergency departments for children) in the United States.[75]
Research
[edit]Scientific work into the prediction of epileptic seizures began in the 1970s. Several techniques and methods have been proposed, but evidence regarding their usefulness is still lacking.[76]
Two promising areas include: (1) gene therapy,[77] and (2) seizure detection and seizure prediction.[78]
Gene therapy for epilepsy consists of employing vectors to deliver pieces of genetic material to areas of the brain involved in seizure onset.[77]
Seizure prediction is a special case of seizure detection in which the developed systems is able to issue a warning before the clinical onset of the epileptic seizure.[76][78]
Computational neuroscience has been able to bring a new point of view on the seizures by considering the dynamical aspects.[79]
References
[edit]- ^ Shorvon S (2009). Epilepsy. OUP Oxford. p. 1. ISBN 9780199560042.
- ^ "Epileptic Seizures - National Library of Medicine". PubMed Health. Retrieved 16 October 2018.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw Berkowitz, Aaron L. (2022). "Seizures & Epilepsy". Clinical Neurology & Neuroanatomy: A Localization-Based Approach (2nd ed.). McGraw Hill. ISBN 978-1260453362.
- ^ Mayo Clinic Staff. "Seizures – Symptoms and causes". Mayo Clinic.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax Abou-Khalil, Bassel W.; Gallagher, Martin J.; Macdonald, Robert L. (2022). "Epilepsies". Bradley and Daroff's Neurology in Clinical Practice (8th ed.). Elsevier. pp. 1614–1663. ISBN 978-0323642613.
- ^ a b c d e f g h Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. (April 2014). "ILAE official report: a practical clinical definition of epilepsy". Epilepsia. 55 (4): 475–482. doi:10.1111/epi.12550. PMID 24730690. S2CID 35958237.
- ^ a b c d e f g h i Wilden JA, Cohen-Gadol AA (August 2012). "Evaluation of first nonfebrile seizures". American Family Physician. 86 (4): 334–340. PMID 22963022.
- ^ a b c d e f g h i j k l m n o p q r s t Winkel, Daniel; Cassimatis, Dimitri (2022). "Episodic Impairment of Consciousness". Bradley and Daroff's Neurology in Clinical Practice (8th ed.). Elsevier. pp. 8–16. ISBN 978-0323642613.
- ^ a b c d Cruickshank, Moira; Imamura, Mari; Booth, Corinne; Aucott, Lorna; Counsell, Carl; Manson, Paul; Scotland, Graham; Brazzelli, Miriam (2022). "Pre-hospital and emergency department treatment of convulsive status epilepticus in adults: an evidence synthesis". Health Technology Assessment. 26 (20): 1–76. doi:10.3310/RSVK2062. ISSN 2046-4924. PMC 8977974. PMID 35333156.
- ^ Ferri FF (2018). Ferri's Clinical Advisor 2019 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 959. ISBN 9780323550765.
- ^ "Epilepsy". World Health Organization. 9 February 2023. Retrieved 4 June 2023.
- ^ Misulis KE, Murray EL (2017). Essentials of Hospital Neurology. Oxford University Press. p. Chapter 19. ISBN 9780190259433.
- ^ a b c d e f g h i j k l m n Ropper, Allan H.; Samuels, Martin A.; Klein, Joshua P.; PrasadPrasad, Sashank (2023). "Epilepsy and Other Seizure Disorders". Adams and Victor's Principles of Neurology (12th ed.). McGraw-Hill. ISBN 978-1264264520.
- ^ a b c Neligan, Aidan; Adan, Guleed; Nevitt, Sarah J; Pullen, Angie; Sander, Josemir W; Bonnett, Laura; Marson, Anthony G (23 January 2023). Cochrane Epilepsy Group (ed.). "Prognosis of adults and children following a first unprovoked seizure". Cochrane Database of Systematic Reviews. 2023 (1): CD013847. doi:10.1002/14651858.CD013847.pub2. PMC 9869434. PMID 36688481.
- ^ a b c Pottkämper, Julia C. M.; Hofmeijer, Jeannette; van Waarde, Jeroen A.; van Putten, Michel J. A. M. (2020). "The postictal state-What do we know?". Epilepsia. 61 (6): 1045–1061. doi:10.1111/epi.16519. ISSN 1528-1167. PMC 7317965. PMID 32396219.
- ^ James W. Wheless, ed. (2009). Advanced therapy in epilepsy. Shelton, Conn.: People's Medical Pub. House. p. 443. ISBN 978-1-60795-004-2.
- ^ Panayiotopoulos CP (2010). A clinical guide to epileptic syndromes and their treatment based on the ILAE classifications and practice parameter guidelines (Rev. 2nd ed.). [London]: Springer. p. 445. ISBN 978-1-84628-644-5.
- ^ Chee, Keanu; Razmara, Ashkaun; Geller, Aaron S.; Harris, William B.; Restrepo, Diego; Thompson, John A.; Kramer, Daniel R. (2022). "The role of the piriform cortex in temporal lobe epilepsy: A current literature review". Frontiers in Neurology. 13: 1042887. doi:10.3389/fneur.2022.1042887. ISSN 1664-2295. PMC 9720270. PMID 36479052.
- ^ Xu, Sui-Yi; Li, Ze-Xing; Wu, Xiao-Wei; Li, Ling; Li, Chang-Xin (5 March 2020). "Frequency and Pathophysiology of Post-Seizure Todd's Paralysis". Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 26: e920751. doi:10.12659/MSM.920751. ISSN 1643-3750. PMC 7075081. PMID 32134903.
- ^ Thurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, Ding D, et al. (September 2011). "Standards for epidemiologic studies and surveillance of epilepsy". Epilepsia. 52 (Suppl 7): 2–26. doi:10.1111/j.1528-1167.2011.03121.x. PMID 21899536. S2CID 8505004.
- ^ Stasiukyniene V, Pilvinis V, Reingardiene D, Janauskaite L (2009). "[Epileptic seizures in critically ill patients]". Medicina. 45 (6): 501–507. doi:10.3390/medicina45060066. PMID 19605972.
- ^ a b Nardone, Raffaele; Brigo, Francesco; Trinka, Eugen (2016). "Acute Symptomatic Seizures Caused by Electrolyte Disturbances". Journal of Clinical Neurology. 12 (1): 21–33. doi:10.3988/jcn.2016.12.1.21. ISSN 1738-6586. PMC 4712283. PMID 26754778.
- ^ a b c Chen, Hsien-Yi; Albertson, Timothy E.; Olson, Kent R. (2015). "Treatment of drug-induced seizures". British Journal of Clinical Pharmacology. 81 (3): 412–419. doi:10.1111/bcp.12720. ISSN 0306-5251. PMC 4767205. PMID 26174744.
- ^ Bauer, Derek; Quigg, Mark (April 2019). "Optimizing Management of Medically Responsive Epilepsy". CONTINUUM: Lifelong Learning in Neurology. 25 (2): 343–361. doi:10.1212/CON.0000000000000709. ISSN 1080-2371. PMID 30921013. S2CID 85563793.
- ^ a b Xixis, Kathryn L.; Samanta, Debopam; Smith, Travis; Keenaghan, Michael (2024), "Febrile Seizure", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28846243, retrieved 1 November 2024
- ^ Graves RC, Oehler K, Tingle LE (January 2012). "Febrile seizures: risks, evaluation, and prognosis". American Family Physician. 85 (2): 149–153. PMID 22335215.
- ^ a b c Chen, Jiayu; Ye, Haijiao; Zhang, Jie; Li, Aihong; Ni, Yaohui (2022). "Pathogenesis of seizures and epilepsy after stroke". Acta Epileptologica. 4 (1): 2. doi:10.1186/s42494-021-00068-8. ISSN 2524-4434.
- ^ a b Zöllner, Johann Philipp; Schmitt, Friedhelm C.; Rosenow, Felix; Kohlhase, Konstantin; Seiler, Alexander; Strzelczyk, Adam; Stefan, Hermann (6 December 2021). "Seizures and epilepsy in patients with ischaemic stroke". Neurological Research and Practice. 3 (1) (published 2021): 63. doi:10.1186/s42466-021-00161-w. ISSN 2524-3489. PMC 8647498. PMID 34865660.
- ^ a b c Englander, Jeffrey; Cifu, David X.; Diaz-Arrastia, Ramon (2014). "Seizures after Traumatic Brain Injury". Archives of Physical Medicine and Rehabilitation. 95 (6): 1223–1224. doi:10.1016/j.apmr.2013.06.002. PMC 4516165. PMID 24862307.
- ^ Hildebrand J (July 2004). "Management of epileptic seizures". Current Opinion in Oncology. 16 (4): 314–317. doi:10.1097/01.cco.0000127720.17558.38. PMID 15187884. S2CID 12828909.
- ^ Sanghvi, Jagruti P.; Rajadhyaksha, Surekha B.; Ursekar, Meher (2004). "Spectrum of congenital CNS malformations in pediatric epilepsy". Indian Pediatrics. 41 (8): 831–838. ISSN 0019-6061. PMID 15347872 – via PubMed.
- ^ Shetty, Jayakara (2015). "Neonatal seizures in hypoxic–ischaemic encephalopathy – risks and benefits of anticonvulsant therapy". Developmental Medicine & Child Neurology. 57 (S3): 40–43. doi:10.1111/dmcn.12724. ISSN 0012-1622. PMID 25800491 – via PubMed.
- ^ a b c Vezzani, Annamaria; Fujinami, Robert S.; White, H. Steve; Preux, Pierre-Marie; Blümcke, Ingmar; Sander, Josemir W.; Löscher, Wolfgang (2015). "Infections, inflammation and epilepsy". Acta Neuropathologica. 131 (2): 211–234. doi:10.1007/s00401-015-1481-5. ISSN 0001-6322. PMC 4867498. PMID 26423537.
- ^ Bhalla D, Godet B, Druet-Cabanac M, Preux PM (June 2011). "Etiologies of epilepsy: a comprehensive review". Expert Review of Neurotherapeutics. 11 (6): 861–876. doi:10.1586/ern.11.51. PMID 21651333. S2CID 21190601.
- ^ a b c Tatti, Roberta; Haley, Melissa S.; Swanson, Olivia K.; Tselha, Tenzin; Maffei, Arianna (15 May 2017). "Neurophysiology and Regulation of the Balance Between Excitation and Inhibition in Neocortical Circuits". Biological Psychiatry. 81 (10): 821–831. doi:10.1016/j.biopsych.2016.09.017. ISSN 1873-2402. PMC 5374043. PMID 27865453.
- ^ a b Chauhan, Pradip; Philip, Shalom Elsy; Chauhan, Girish; Mehra, Simmi (4 April 2022), Department of Pathophysiology, Medical University of Lublin, Lublin, Poland; J. Czuczwar, Stanislaw (eds.), "The Anatomical Basis of Seizures", Epilepsy, Exon Publications, pp. 15–24, doi:10.36255/exon-publications-epilepsy-anatomical-basis, ISBN 978-0-6453320-4-9, PMID 35605083, retrieved 31 October 2024
{{citation}}: CS1 maint: multiple names: editors list (link) - ^ a b c d Treiman, David M. (2001). "GABAergic Mechanisms in Epilepsy". Epilepsia. 42 (s3): 8–12. doi:10.1046/j.1528-1157.2001.042suppl.3008.x. ISSN 0013-9580. PMID 11520315 – via Wiley Online Library.
- ^ a b c d e f Sarlo, Gabrielle L.; Holton, Kathleen F. (2021). "Brain concentrations of glutamate and GABA in human epilepsy: A review". Seizure - European Journal of Epilepsy. 91: 213–227. doi:10.1016/j.seizure.2021.06.028. PMID 34233236 – via Elsevier Science Direct.
- ^ Wei F, Yan LM, Su T, He N, Lin ZJ, Wang J, et al. (August 2017). "Ion Channel Genes and Epilepsy: Functional Alteration, Pathogenic Potential, and Mechanism of Epilepsy". Neuroscience Bulletin. 33 (4): 455–477. doi:10.1007/s12264-017-0134-1. PMC 5567559. PMID 28488083.
- ^ a b c Bromfield, Edward B.; Cavazos, José E.; Sirven, Joseph I. (2006), "Basic Mechanisms Underlying Seizures and Epilepsy", An Introduction to Epilepsy [Internet], American Epilepsy Society, retrieved 31 October 2024
- ^ a b c Goldberg EM, Coulter DA (May 2013). "Mechanisms of epileptogenesis: a convergence on neural circuit dysfunction". Nature Reviews. Neuroscience. 14 (5): 337–349. doi:10.1038/nrn3482. PMC 3982383. PMID 23595016.
- ^ a b c d Dingledine, Ray; Varvel, Nicholas H.; Dudek, F. Edward (2014), Scharfman, Helen E.; Buckmaster, Paul S. (eds.), "When and How Do Seizures Kill Neurons, and Is Cell Death Relevant to Epileptogenesis?", Issues in Clinical Epileptology: A View from the Bench, vol. 813, Dordrecht: Springer Netherlands, pp. 109–122, doi:10.1007/978-94-017-8914-1_9, ISBN 978-94-017-8913-4, PMC 4624106, PMID 25012371
- ^ a b Jerome Engel Jr.; Timothy A. Pedley, eds. (2008). Epilepsy : a comprehensive textbook (2nd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 483. ISBN 978-0-7817-5777-5.
- ^ a b c d e f g h i j Rowland, Kate; Lambert, Carl Earl (1 May 2022). "Evaluation After a First Seizure in Adults". American Family Physician. 105 (5): 507–513. ISSN 1532-0650. PMID 35559631.
- ^ Peeters SY, Hoek AE, Mollink SM, Huff JS (April 2014). "Syncope: risk stratification and clinical decision making". Emergency Medicine Practice. 16 (4): 1–22, quiz 22–3. PMID 25105200.
- ^ Biasiucci, Andrea; Franceschiello, Benedetta; Murray, Micah M. (4 February 2019). "Electroencephalography". Current Biology. 29 (3): R80–R85. Bibcode:2019CBio...29..R80B. doi:10.1016/j.cub.2018.11.052. ISSN 1879-0445. PMID 30721678.
- ^ Chang, Bernard S.; Lowenstein, Daniel H. (14 January 2003). "Practice parameter: Antiepileptic drug prophylaxis in severe traumatic brain injury: Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 60 (1): 10–16. doi:10.1212/01.WNL.0000031432.05543.14. ISSN 0028-3878. PMID 12525711.
- ^ Torbic, Heather; Forni, Allison A.; Anger, Kevin E.; Degrado, Jeremy R.; Greenwood, Bonnie C. (1 May 2013). "Use of antiepileptics for seizure prophylaxis after traumatic brain injury". American Journal of Health-System Pharmacy. 70 (9): 759–766. doi:10.2146/ajhp120203. ISSN 1079-2082. PMID 23592358.
- ^ Greenhalgh, Janette; Weston, Jennifer; Dundar, Yenal; Nevitt, Sarah; Marson, Anthony (28 April 2020). "Antiepileptic drugs as prophylaxis for postcraniotomy seizures". The Cochrane Database of Systematic Reviews. 4 (4): CD007286. doi:10.1002/14651858.CD007286.pub5. ISSN 1469-493X. PMC 7195181. PMID 32343399.
- ^ Chang, Richard S.; Leung, William Cy; Vassallo, Michael; Sykes, Lucy; Battersby Wood, Emma; Kwan, Joseph (7 February 2022). "Antiepileptic drugs for the primary and secondary prevention of seizures after stroke". The Cochrane Database of Systematic Reviews. 2022 (2): CD005398. doi:10.1002/14651858.CD005398.pub4. ISSN 1469-493X. PMC 8819727. PMID 35129214.
- ^ Marigold R, Günther A, Tiwari D, Kwan J (June 2013). "Antiepileptic drugs for the primary and secondary prevention of seizures after subarachnoid haemorrhage". The Cochrane Database of Systematic Reviews. 2013 (6): CD008710. doi:10.1002/14651858.CD008710.pub2. hdl:10722/194540. PMC 6885058. PMID 23740537.
- ^ Greenhalgh J, Weston J, Dundar Y, Nevitt SJ, Marson AG (April 2020). "Antiepileptic drugs as prophylaxis for postcraniotomy seizures". The Cochrane Database of Systematic Reviews. 4 (4): CD007286. doi:10.1002/14651858.CD007286.pub5. PMC 7195181. PMID 32343399.
- ^ Ratilal BO, Pappamikail L, Costa J, Sampaio C (June 2013). "Anticonvulsants for preventing seizures in patients with chronic subdural haematoma". The Cochrane Database of Systematic Reviews. 2013 (6): CD004893. doi:10.1002/14651858.CD004893.pub3. PMC 7388908. PMID 23744552.
- ^ a b Offringa M, Newton R, Nevitt SJ, Vraka K (June 2021). "Prophylactic drug management for febrile seizures in children". The Cochrane Database of Systematic Reviews. 2021 (6): CD003031. doi:10.1002/14651858.CD003031.pub4. PMC 8207248. PMID 34131913.
- ^ a b c d e Asadi-Pooya, Ali A.; Hosseini, Seyed Ali; Hashemizadeh Fard Haghighi, Leila; Asadi-Pooya, Hanieh (2022). "Seizure first aid for people with epilepsy: opinions and knowledge of caregivers and healthcare professionals". Seizure. 102: 1–5. doi:10.1016/j.seizure.2022.09.007. ISSN 1532-2688. PMID 36130455 – via PubMed.
- ^ Al-Mufti F, Claassen J (October 2014). "Neurocritical care: status epilepticus review". Critical Care Clinics. 30 (4): 751–764. doi:10.1016/j.ccc.2014.06.006. PMID 25257739.
- ^ De Waele L, Boon P, Ceulemans B, Dan B, Jansen A, Legros B, et al. (December 2013). "First line management of prolonged convulsive seizures in children and adults: good practice points". Acta Neurologica Belgica. 113 (4): 375–380. doi:10.1007/s13760-013-0247-x. hdl:1854/LU-4182539. PMID 24019121. S2CID 17641491.
- ^ Chhabra, Ridhi; Gupta, Rachna; Gupta, Lalit K (2021). "Intranasal midazolam versus intravenous/rectal benzodiazepines for acute seizure control in children: A systematic review and meta-analysis". Epilepsy & Behavior. 125: 108390. doi:10.1016/j.yebeh.2021.108390. ISSN 1525-5050. PMID 34740090 – via Elsevier Science Direct.
- ^ a b c d e f Liu, Gerald; Slater, Nicole; Perkins, Allen (15 July 2017). "Epilepsy: Treatment Options". American Family Physician. 96 (2): 87–96. ISSN 1532-0650. PMID 28762701.
- ^ a b "Epilepsy". Fact Sheets. World Health Organization. October 2012. Archived from the original on 11 March 2016. Retrieved 24 January 2013.
- ^ Matern, Tyson S.; DeCarlo, Rebecca; Ciliberto, Michael A.; Singh, Rani K. (2021). "Palliative Epilepsy Surgery Procedures in Children". Seminars in Pediatric Neurology. 39: 100912. doi:10.1016/j.spen.2021.100912. ISSN 1558-0776. PMID 34620461 – via PubMed.
- ^ a b Doherty MJ, Haltiner AM (January 2007). "Wag the dog: skepticism on seizure alert canines". Neurology. 68 (4): 309. CiteSeerX 10.1.1.1003.1543. doi:10.1212/01.wnl.0000252369.82956.a3. PMID 17242343. S2CID 33328776.
- ^ Lattanzi, Simona; Trinka, Eugen; Striano, Pasquale; Rocchi, Chiara; Salvemini, Sergio; Silvestrini, Mauro; Brigo, Francesco (2021). "Highly Purified Cannabidiol for Epilepsy Treatment: A Systematic Review of Epileptic Conditions Beyond Dravet Syndrome and Lennox–Gastaut Syndrome". CNS Drugs. 35 (3): 265–281. doi:10.1007/s40263-021-00807-y. PMC 8005394. PMID 33754312.
- ^ Elliott, Jesse; DeJean, Deirdre; Clifford, Tammy; Coyle, Doug; Potter, Beth K.; Skidmore, Becky; Alexander, Christine; Repetski, Alexander E.; Shukla, Vijay; McCoy, Bláthnaid; Wells, George A. (2020). "Cannabis-based products for pediatric epilepsy: An updated systematic review". Seizure. 75: 18–22. doi:10.1016/j.seizure.2019.12.006. ISSN 1532-2688. PMID 31865133 – via PubMed.
- ^ Martin-McGill, Kirsty J.; Bresnahan, Rebecca; Levy, Robert G.; Cooper, Paul N. (24 June 2020). "Ketogenic diets for drug-resistant epilepsy". The Cochrane Database of Systematic Reviews. 2020 (6): CD001903. doi:10.1002/14651858.CD001903.pub5. ISSN 1469-493X. PMC 7387249. PMID 32588435.
- ^ Devi, Nagita; Madaan, Priyanka; Kandoth, Nidhun; Bansal, Dipika; Sahu, Jitendra Kumar (2023). "Efficacy and Safety of Dietary Therapies for Childhood Drug-Resistant Epilepsy: A Systematic Review and Network Meta-analysis". JAMA Pediatrics. 177 (3): 258–266. doi:10.1001/jamapediatrics.2022.5648. PMC 9887534. PMID 36716045.
- ^ Bonnett LJ, Tudur-Smith C, Williamson PR, Marson AG (December 2010). "Risk of recurrence after a first seizure and implications for driving: further analysis of the Multicentre study of early Epilepsy and Single Seizures". BMJ. 341: c6477. doi:10.1136/bmj.c6477. PMC 2998675. PMID 21147743.
- ^ Neligan A, Hauser WA, Sander JW (2012). "The epidemiology of the epilepsies". Epilepsy. Handbook of Clinical Neurology. Vol. 107. pp. 113–33. doi:10.1016/B978-0-444-52898-8.00006-9. ISBN 9780444528988. PMID 22938966.; Sander JW, Shorvon SD (November 1996). "Epidemiology of the epilepsies". Journal of Neurology, Neurosurgery, and Psychiatry. 61 (5): 433–443. doi:10.1136/jnnp.61.5.433. PMC 1074036. PMID 8965090.
- ^ a b c Gavvala JR, Schuele SU (December 2016). "New-Onset Seizure in Adults and Adolescents: A Review". JAMA. 316 (24): 2657–2668. doi:10.1001/jama.2016.18625. PMID 28027373.
- ^ Camfield P, Camfield C (June 2015). "Incidence, prevalence and aetiology of seizures and epilepsy in children". Epileptic Disorders. 17 (2): 117–123. doi:10.1684/epd.2015.0736. PMID 25895502. S2CID 20719640.
- ^ a b Magiorkinis E, Sidiropoulou K, Diamantis A (January 2010). "Hallmarks in the history of epilepsy: epilepsy in antiquity". Epilepsy & Behavior. 17 (1): 103–108. doi:10.1016/j.yebeh.2009.10.023. PMID 19963440. S2CID 26340115.
- ^ a b c d Ali R, Connolly ID, Feroze AH, Awad AJ, Choudhri OA, Grant GA (June 2016). "Epilepsy: A Disruptive Force in History". World Neurosurgery. 90: 685–690. doi:10.1016/j.wneu.2015.11.060. PMID 26709155.
- ^ Meador KJ, Loring DW, Flanigin HF (January 1989). "History of epilepsy surgery". Journal of Epilepsy. 2 (1): 21–25. doi:10.1016/0896-6974(89)90054-6. ISSN 0896-6974.
- ^ National Institute for Health and Clinical Excellence (January 2012). "Chapter 1: Introduction" (PDF). The Epilepsies: The diagnosis and management of the epilepsies in adults and children in primary and secondary care. National Clinical Guideline Centre. pp. 21–28. Archived (PDF) from the original on 16 December 2013.
- ^ Martindale JL, Goldstein JN, Pallin DJ (February 2011). "Emergency department seizure epidemiology". Emergency Medicine Clinics of North America. 29 (1): 15–27. doi:10.1016/j.emc.2010.08.002. PMID 21109099.
- ^ a b Litt B, Echauz J (May 2002). "Prediction of epileptic seizures". The Lancet. Neurology. 1 (1): 22–30. doi:10.1016/S1474-4422(02)00003-0. PMID 12849542. S2CID 10109539.
- ^ a b Walker MC, Schorge S, Kullmann DM, Wykes RC, Heeroma JH, Mantoan L (September 2013). "Gene therapy in status epilepticus". Epilepsia. 54 (Suppl 6): 43–45. doi:10.1111/epi.12275. PMID 24001071. S2CID 13942394.
- ^ a b Mormann F, Andrzejak RG, Elger CE, Lehnertz K (February 2007). "Seizure prediction: the long and winding road". Brain. 130 (Pt 2): 314–333. doi:10.1093/brain/awl241. PMID 17008335.
- ^ Depannemaecker D, Destexhe A, Jirsa V, Bernard C (August 2021). "Modeling seizures: From single neurons to networks". Seizure. 90: 4–8. doi:10.1016/j.seizure.2021.06.015. PMID 34219016. S2CID 235468072.
